Cranial nerve tests are essential for assessing the function of the 12 cranial nerves, which control critical sensory and motor functions. These tests help diagnose neurological conditions by evaluating vision, hearing, smell, and muscle strength. Early detection of abnormalities can guide timely treatment and improve patient outcomes. Standardized methods ensure accuracy and reliability in clinical practice.
1.1 Overview of Cranial Nerves and Their Functions
The 12 cranial nerves regulate vital functions, including vision, hearing, smell, taste, and motor control. CN I (Olfactory) manages smell, while CN II (Optic) controls vision. CN III, IV, VI govern eye movements, and CN VII (Facial) controls facial expressions. CN IX, X manage swallowing and taste, while CN XI, XII regulate neck and tongue movements. Each nerve has distinct roles, ensuring proper sensory and motor functions.
1.2 Importance of Cranial Nerve Testing in Clinical Practice
Cranial nerve testing is crucial for diagnosing neurological disorders and assessing nerve function. It helps identify deficits in vision, hearing, taste, and motor skills. Early detection of abnormalities enables timely intervention, improving patient outcomes. These tests guide further diagnostic steps, such as imaging or referrals, ensuring accurate diagnoses and targeted treatments. Regular assessments prevent complications and aid in monitoring disease progression or recovery.

Preparation for Cranial Nerve Examination
Preparation involves washing hands, introducing yourself, obtaining consent, and positioning the patient comfortably. Ensure necessary equipment is ready, and the environment is conducive for accurate assessment.
2.1 Equipment Needed for Testing
Essential equipment includes a Snellen chart for visual acuity, a 256Hz tuning fork for hearing tests, and aromatic substances for olfactory assessment. Additional tools like a penlight, gloves, and a reflex hammer may be required. Ensure all items are sterilized and ready to facilitate smooth and effective cranial nerve testing.
2.2 Patient Positioning and Comfort
Position the patient comfortably in a chair, seated upright with feet flat on the floor. Ensure the patient is at eye level to the examiner for accurate assessments. Provide a supportive environment, minimizing distractions. Comfort is key to obtaining reliable results during cranial nerve testing.
Begin by introducing yourself, confirming the patient’s identity, and explaining the purpose of the examination. Obtain informed consent, ensuring the patient understands the procedures involved. Address any concerns or discomfort the patient may have to establish trust and cooperation. This initial interaction is crucial for a smooth and effective cranial nerve assessment.
Testing the Olfactory Nerve (CN I)
Assess the olfactory nerve by testing the patient’s ability to detect and identify specific odors, such as coffee or peppermint, using one nostril at a time.
3.1 Smell Testing Techniques
Smell testing involves using standardized odorants like coffee, cloves, or peppermint. Each nostril is tested separately, with the patient identifying the scent. This method evaluates the olfactory nerve’s function and detects anosmia or hyposmia. Patients should close their eyes to focus on smell perception. Results are compared bilaterally to ensure accuracy and reliability in clinical assessment.
3.2 Interpretation of Olfactory Nerve Test Results
Normal results indicate the patient can identify odors bilaterally. Unilateral or bilateral anosmia suggests olfactory nerve dysfunction. Hyposmia, or reduced smell, may indicate partial damage. Abnormal findings warrant further investigation, such as MRI, to rule out conditions like trauma, tumors, or infections. Accurate interpretation is crucial for diagnosing and managing olfactory nerve-related disorders effectively in clinical practice.

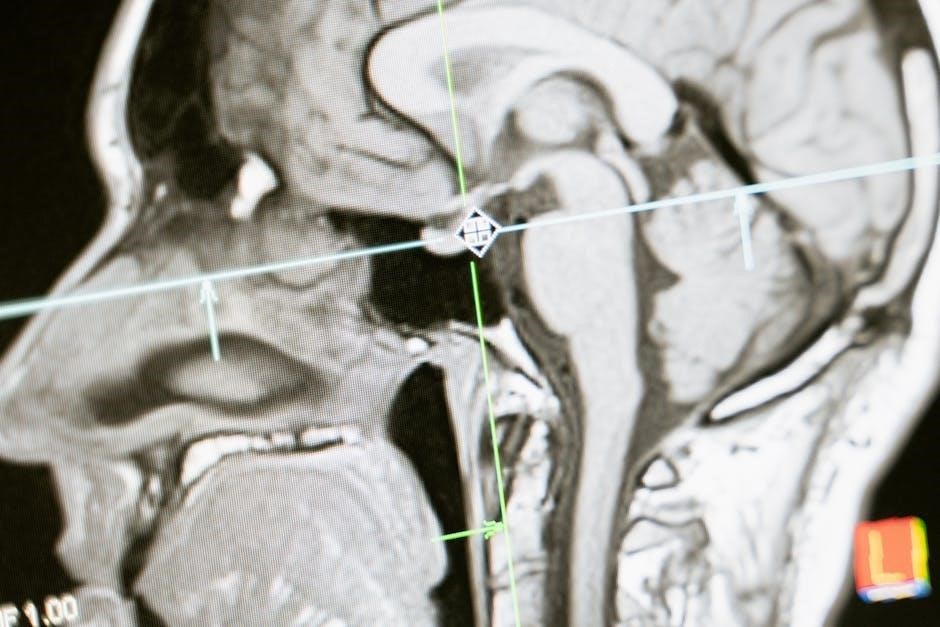
Testing the Optic Nerve (CN II)
Assess visual acuity using Snellen charts, evaluate pupillary light reflex, and perform fundoscopic exams to inspect the optic disc and retina for abnormalities or signs of disease.
4.1 Visual Acuity Tests (e.g., Snellen Chart)
Visual acuity tests, such as the Snellen chart, measure the sharpness of a patient’s vision. The patient reads letters at 20 feet, with results indicating the smallest line they can see clearly. This test is crucial for detecting impairments in central vision and diagnosing conditions like myopia or optic nerve disorders. Abnormal results may warrant further investigation.
4.2 Pupillary Light Reflex Assessment
The pupillary light reflex assesses the optic nerve’s function by shining a penlight into each eye. A normal response is pupil constriction in both the tested and contralateral eye. Absent or abnormal reactions may indicate optic nerve damage or neurological disorders. This test is crucial for detecting conditions like optic neuritis or severe vision impairment early in clinical evaluation.
4.3 Fundoscopic Examination
The fundoscopic exam uses an ophthalmoscope to inspect the optic disc, retina, and blood vessels. It evaluates optic nerve health, checking for signs like disc swelling, pallor, or hemorrhages. Abnormal findings may indicate conditions such as papilledema, optic atrophy, or retinal damage, providing crucial insights into neurological and ocular health during cranial nerve assessments.
Testing the Oculomotor, Trochlear, and Abducens Nerves (CN III, IV, VI)
These nerves control eye movements and pupillary reactions. The oculomotor nerve (CN III) manages most eye movements and pupillary constriction. The trochlear (CN IV) and abducens (CN VI) nerves regulate superior oblique and lateral rectus muscle function, respectively. Testing involves assessing eye alignment, tracking, and reflexes to identify deficits or paralysis affecting ocular motility.
5.1 Assessing Eye Movements and Alignment
Assess eye movements by asking the patient to track an object in an H-shaped pattern. Observe for smooth pursuit, nystagmus, or limitations. Check alignment with the cover-uncover test. Evaluate version and vergence movements. Ensure the eyes move conjugately in all directions. Note any diplopia or muscle weakness. This step helps identify deficits in CN III, IV, or VI function, guiding further diagnostic steps.
5.2 Testing Pupillary Reactions
Assess pupillary reactions using the pupillary light reflex. Shine a light into one eye and observe bilateral constriction. Test each eye individually. Note the presence of anisocoria or sluggish reactions. Evaluate consensual responses to ensure CN III and IV integrity. Abnormalities may indicate nerve dysfunction or underlying conditions affecting autonomic pathways. Accurate testing aids in diagnosing neurological deficits promptly and effectively.
Testing the Trigeminal Nerve (CN V)
Assess sensory function with light touch and pain tests on the face. Evaluate motor strength by testing jaw muscle resistance. Check the corneal reflex for integrity.
6.1 Sensory Testing (e.g., Light Touch, Pain)
Sensory testing involves assessing light touch and pain perception across the trigeminal nerve’s three branches. Use a soft brush or cotton swab for light touch and a sterile pin for pain. Compare bilateral responses to detect abnormalities like hypoesthesia or hyperesthesia, which may indicate nerve damage or dysfunction.
6.2 Motor Testing (e.g., Jaw Muscle Strength)
Assess motor function by evaluating jaw muscle strength and movement. Palpate the masseter and temporalis muscles while the patient clenches their jaw. Test resistance by asking the patient to open their mouth against gentle downward pressure. Asymmetry, weakness, or pain may indicate trigeminal nerve dysfunction or underlying musculoskeletal issues.
6.3 Corneal Reflex Evaluation
Evaluate the corneal reflex by gently touching the cornea with a soft object or cotton swab. Observe bilateral blinking, indicating intact trigeminal (afferent) and facial (efferent) pathways. Absence or diminished reflex suggests nerve dysfunction. Ensure patient comfort and explain the procedure to avoid voluntary responses. This test is crucial for assessing cranial nerve V function and integrity.

Testing the Facial Nerve (CN VII)
Evaluate the corneal reflex by gently touching the cornea with a soft object or cotton swab. Observe bilateral blinking, indicating intact trigeminal (afferent) and facial (efferent) pathways. Absence or diminished reflex suggests nerve dysfunction. Ensure patient comfort and explain the procedure to avoid voluntary responses. This test is crucial for assessing cranial nerve V function and integrity.
7.1 Facial Muscle Strength and Symmetry
Assess facial muscle strength by asking the patient to perform actions like raising eyebrows, puffing cheeks, smiling, and closing eyes tightly. Observe symmetry and strength in upper and lower facial muscles. Note any weakness, asymmetry, or inability to perform movements, which may indicate facial nerve dysfunction. This evaluation helps identify potential nerve damage or paralysis affecting motor function.
7.2 Taste Testing
Taste testing evaluates the facial nerve’s (CN VII) role in taste sensation. Apply sweet, sour, salty, or bitter substances to the anterior tongue bilaterally. Ask the patient to identify each taste with eyes closed. This assesses the chorda tympani branch, which mediates taste for the anterior two-thirds of the tongue. Ensure substances are non-allergenic and instructions are clear for accurate results.
7.3 Stapedius Reflex Assessment
The stapedius reflex assesses the facial nerve’s (CN VII) branch to the stapedius muscle. It involves measuring the reflexive contraction of the stapedius muscle in response to loud sounds. This is tested using tympanometry or a tuning fork. The absence or reduction of the reflex may indicate facial nerve dysfunction or hearing abnormalities. It is crucial for diagnosing hearing-related conditions and nerve damage.
Testing the Vestibulocochlear Nerve (CN VIII)
This nerve governs hearing and balance. Testing includes Weber and Rinne tests to assess hearing loss and vestibular function tests like the turning test to evaluate balance disturbances.
8.1 Weber and Rinne Tests
The Weber test involves placing a tuning fork on the forehead to assess lateralization of sound, helping differentiate conductive from sensorineural hearing loss. The Rinne test compares bone conduction to air conduction by placing the fork on the mastoid process and then near the ear canal, determining if air conduction is greater, indicating normal hearing or a sensorineural issue.
8.2 Vestibular Function Tests (e.g., Turning Test)
Vestibular function tests assess balance and equilibrium. The turning test involves observing nystagmus and balance during slow head turns. Positive results indicate vestibular dysfunction. Additional tests like the Dix-Hallpike maneuver evaluate positional vertigo. These assessments help diagnose inner ear or central nervous system disorders affecting the vestibulocochlear nerve, guiding appropriate management strategies for patients with balance-related symptoms.

Testing the Glossopharyngeal Nerve (CN IX)
The glossopharyngeal nerve controls swallowing, taste on the posterior tongue, and the gag reflex. Testing involves swallowing assessment, gag reflex evaluation, and taste testing to identify dysfunction.
9.1 Swallowing and Gag Reflex Assessment
Assessing the gag reflex involves gently touching the posterior pharynx or uvula with a cotton swab. The patient’s ability to swallow water or other liquids is observed. A diminished or absent gag reflex may indicate nerve damage, while difficulty swallowing suggests dysphagia, requiring further evaluation to rule out neurological or structural issues.
9.2 Taste Testing on the Posterior Tongue
Taste testing on the posterior tongue evaluates the glossopharyngeal nerve. Apply sweet, sour, salty, or bitter solutions to the back of the tongue using a cotton swab. Assess the patient’s ability to identify each taste. Impaired taste perception may indicate nerve dysfunction, guiding further diagnostic steps to address potential neurological conditions affecting cranial nerve IX.
Testing the Vagus Nerve (CN X)
Assess swallowing, gag reflex, and voice quality. Test cough strength and observe soft palate movement; These tests evaluate motor and sensory functions of the vagus nerve.
10.1 Soft Palate and Uvula Inspection
Examine the soft palate and uvula for symmetry and movement. Ask the patient to say “ahh” to observe elevation. Note any deviations or paralysis, which may indicate vagus nerve dysfunction. This assessment evaluates the nerve’s motor function, crucial for swallowing and speech. Abnormalities may suggest neurological conditions requiring further investigation. Detailed observation ensures accurate clinical interpretation.
10.2 Cough and Voice Assessment
Assess the patient’s cough strength and voice quality. A weak or hoarse voice may indicate vagus nerve impairment. Ask the patient to cough and speak to evaluate motor function. Note any breathiness or nasal resonance, which could suggest dysfunction. This test is crucial for identifying neurological issues affecting the vagus nerve, guiding further diagnostic steps and treatment plans effectively.

Testing the Accessory Nerve (CN XI)
Assess the sternocleidomastoid and trapezius muscles for strength and symmetry. Test resistance during head rotation and shoulder shrug to evaluate motor function of the accessory nerve.
11.1 Sternocleidomastoid and Trapezius Muscle Testing
Assess the sternocleidomastoid by asking the patient to rotate their head against resistance. Evaluate the trapezius by having the patient shrug their shoulders against resistance. Observe for symmetry, strength, and range of motion. Note any muscle atrophy, weakness, or involuntary movements. These tests help identify accessory nerve dysfunction, which may manifest as difficulty turning the head or elevating the shoulders.

Testing the Hypoglossal Nerve (CN XII)
12.1 Tongue Protrusion and Movement Assessment
Assess tongue protrusion, movement, and symmetry. Observe for atrophy, fasciculations, or deviation. Abnormalities may indicate hypoglossal nerve dysfunction, affecting speech and swallowing abilities.
Instruct the patient to protrude their tongue and move it side-to-side. Assess symmetry, strength, and coordination. Note any atrophy, fasciculations, or deviation from the midline. Ask the patient to push their tongue against the inside of each cheek to test lateral movement. Abnormal findings, such as weakness or tremors, may indicate hypoglossal nerve dysfunction, potentially affecting speech and swallowing functions.
Interpretation of Cranial Nerve Test Results
Accurate interpretation of cranial nerve test results is crucial for diagnosing neurological disorders. Abnormal findings, such as weakness or sensory loss, guide further investigations and treatment plans effectively.
13.1 Clinical Implications of Abnormal Findings
Abnormal cranial nerve test results may indicate neurological deficits, such as hearing loss, vision impairment, or facial weakness. These findings can suggest conditions like Bell’s palsy, Lyme disease, or tumors. Early detection allows for timely intervention, improving patient outcomes. Clinicians must correlate test results with patient history and imaging to guide appropriate management and referrals for specialized care when necessary.
13.2 Referral and Further Diagnostic Steps
Abnormal cranial nerve test results may necessitate referral to a neurologist or ENT specialist. Further diagnostics, such as MRI or CT scans, can identify structural abnormalities. Nerve conduction studies or electromyography may be recommended for detailed nerve function assessment. Timely referrals ensure comprehensive evaluation and appropriate treatment, addressing underlying conditions effectively while monitoring recovery or disease progression.



